Patients with difficult intravenous access
Version 1: January 2024
Patients with difficult intravenous access (DIVA) have reduced visible, palpable, quality or number of peripheral veins (1-25). Repeated or prolonged administration of intravenous therapies may result in a patient developing DIVA, making future venous access painful and distressing for the patient and family (1). DIVA considerably challenges first insertion success of peripheral cannulation without the employment of advanced techniques or technology by competent clinicians (26, 27). Patients with DIVA also provide considerable technical and time-consuming challenges for clinicians, as well as reduced efficiency and increased costs at a system level (28-32). Furthermore, insertion of a central venous access device (CVAD) may be appropriate if long-term therapy is required.
Approximately 8% - 12% of adult patients (3, 13, 33) and up to 24% – 35% (14, 20) in the perioperative and emergency departments have DIVA. In the paediatric patient population, DIVA rates vary from 9% (34) to 38% (10). The proportion of patients with DIVA in the cancer setting is currently unknown.
CNSA advocates for standardised, evidence based assessment of all patients prior to PIVC insertion, for early identification and management of DIVA. The aim is to preserve vein health of every patient.
Refer to algorithm below: Management pathway for insertion of Peripheral Intavenous Cannula (PIVC) incorporating Difficult Venous Access (DIVA) (for peripherally compatible infusates)
POSITION STATEMENT: Peripheral intravenous cannula insertion procedure using assistive visual technology including ultrasound and near infrared technology
As a part of developing these guidelines, we have prepared a position statement on Peripheral intravenous cannula insertion procedure using assistive visual technology including ultrasound and near infrared technology
Purpose: To provide evidence-based statements to inform safe, patient focused, standardised PIVC insertion procedures using assistive visual technology including ultrasound (US) or near infrared (NIR) technology.
TERMINOLOGY
Common language facilitates communication between professional and organisations, the translation of evidence into clinical practice, data sharing, and research. CNSA, eviQ and eviQ Education are leading vascular access management and education in cancer care in Australia utilizing common, contemporary terminology (Table 1).
Table 1: CVAD terminology
SUMMARY OF RECOMMENDATIONS
Standard venous status assessment
1. CNSA recommends that clinicians complete a standardised, concise venous status assessment on all patients prior to commencing intravenous therapy to pre-emptively and consistently identify adult and paediatric patients with DIVA (3, 16, 31) including:
- Vein palpability (1, 17, 20, 26, 27, 29, 35-43) GRADE IV
- Vein visibility (1, 17, 20, 26, 27, 29, 35-43) GRADE IV
- History of difficult access or use of advanced strategies to obtain vascular access (1, 13, 30, 31, 38-40, 44-52) including self-identification of their DIVA status (14, 45, 53-55) GRADE IV
2. CNSA recommends an evidence-based venous status assessment tool is documented in workplace procedures to standardise clinical management (40). GRADE IV
3. CNSA recommends a patient’s DIVA status is highlighted in a centralised location in the patient’s health record and is discussed with the patient and family for appropriate future management. GRADE CC
Identification of patients with DIVA
4. CNSA recommends if a patient has at least two of the three following risks factors:
- reduced palpability or visibility of peripheral veins for the prescribed therapy, frequency and duration
- history of difficult intravenous access or self-identification of difficulty by the patient
- previous use of advanced strategies for peripheral intravenous cannula insertion documented in the health record or verbalised by the patient
Then to proceed with:
- DIVA status is documented in the patient health record, discussed with the patient and family, and
- Proceed directly to DIVA management.GRADE CC
5. CNSA recommends completing a comprehensive assessment of DIVA related factors if a clinician is uncertain or the assessment is unclear including:
- Patient related factors: patient preference, vein characteristics, body mass index, diagnoses, age, sex, acuity. NB. Age related variables for paediatric (prematurity and age) and adult (elderly, frail) patients are also detailed (2, 3, 6, 7, 10, 12, 17-19, 24-26, 28, 31, 33, 34, 56-61) GRADE IV
- Therapy related factors: prior chemotherapy administration, previous VAD related complications (2, 4, 11, 13, 20, 21, 34, 51, 57, 58, 62, 63) GRADE IV
- Clinician related factors: experience, skill, confidence (13, 16, 33, 51, 56, 59, 60, 64) GRADE IV
- Workplace related factors: training and education, equipment, and technology (20, 65, 66) GRADE IV
Management of patients with DIVA
6. CNSA recommends the management of adult and paediatric patients with DIVA is performed by educated and competent clinicians (40, 66-69). GRADE IV
7. CNSA recommends advanced management of adults and paediatric patients with DIVA is implemented at the outset and not as a rescue strategy after failed PIVC insertion attempts (3, 20, 70). GRADE Ib
- Advanced management includes:
- 7.1 Patient related: patient preparation for the procedure and care during the dwell time including -
- Education and communication regarding the procedure and dwell time, risks and benefits, what to expect, to report and to whom, and additionally in written form for (46, 66, 68, 71). GRADE IV
- Preparation: communication and education about the procedure, adequate hydration, warmth, relaxation techniques, appropriate pain and anxiety management as required e.g. topical/ subdermal anaesthesia, child life specialists, distraction, virtual reality, socially assistive robots (46, 64, 66, 68, 71-92). GRADE III
- Post procedure: application of cold pack after the procedure for comfort if required, education to reinforce what to report, when and to whom, (46, 66, 68, 71). GRADE IV
- 7.2 Imaging technology:
- Use imaging technology (46, 50, 57, 93, 94) during the insertion procedure, for example
- ultrasound (3, 4, 13, 20, 27, 28, 30, 33, 35, 37, 39-41, 43, 44, 46, 47, 52, 53, 58, 63, 69, 70, 95-100) GRADE Ib OR
- NIR or IR (46, 70, 90, 95, 101-105) GRADE Ib
- Clinicians complete standardised, evidence based theoretical education and practical simulation, assessment of knowledge and practical skills, post supervised successful, independent practice attempts and competency is attained (106). GRADE IV
- Use imaging technology (46, 50, 57, 93, 94) during the insertion procedure, for example
- 7.3 Clinician related:
- Referral to vascular access team or expert (3, 17, 27, 31, 36, 46, 57, 95, 107-109), for ultrasound guided insertion (39, 49) GRADE Ib
- Insertion in the forearm, avoiding areas of flexion (13, 110), alternating arms for ongoing SACTs (111). GRADE IV
- Topical application of heat prior to PIVC insertion procedure (112, 113), not for vein assessment GRADE III
- Limit the number of attempts per clinician (10, 14, 17, 48) for example:
- If after 1 failed attempt, if the clinician is not 80% confident (114) about a successful 2nd attempt, then do not proceed with 2nd attempt and escalate to more experienced vascular access clinician
- If after 1 attempt (6) and the clinician is confident in their skills and patient’s venous status, then a 2nd attempt may be made
- maximum total number of 3 IV attempts with referral to more experienced clinician (6, 10, 17, 57, 58, 95)
- paediatric patients – 0 - 2 attempts by a clinician and early referral experienced clinician (70) or PICC for ≥2 failed PIVC attempts with competent inserters and visual technology e.g. ultrasound (70) GRADE Ib
- 7.4 Product related:
- Increased cannula length when deeper veins are accessed using ultrasound (3, 38, 50, 115) so at least 2.75cm and ideally two thirds of the cannula resides within the vein (44, 116, 117) (Table 2). GRADE IV
- Peripheral venous cannula with guide wire (30, 43, 48). GRADE IV
- 7.1 Patient related: patient preparation for the procedure and care during the dwell time including -
For paediatric patients: consider ultrasound guided-PIVC insertion (29) and appropriate pain and anxiety management (17, 118-122) GRADE III
 Table 2: Catheter size and length to vein scale
Table 2: Catheter size and length to vein scale
1. PATIENTS WITH DIFFICULT INTRAVENOUS ACCESS
1.1 Summary of evidence
Patients experience of DIVA
Patients with DIVA use words such as horrible, anxiety, distressing, frightening, dread, fear and distress to describe the insertion procedures, and often experience multiple painful attempts, for example ten or more (32, 66, 123). Communication and education were poor, for example they were not told what to do if problems developed (66).
Identification of patients with DIVA
Authors identify over 25 patient, therapy, clinician, and workplace-related factors that potentially impact the health of peripheral veins in both adult and paediatric patients and contribute to DIVA. Different terminology is used to describe their tools including scale, algorithm, score, and instrument. The term tool will be used in this review. Also the majority of clinicians (84%) report that they do not use a DIVA assessment tool and there was no standardised management in their workplace (16).
Optimal DIVA management
This systematic review identified core clinical practices for optimal DIVA management. Standardised assessment of all patients prior to commencing intravenous therapy is required to pre-emptively and consistently identify patients with DIVA (3, 16, 31) to ensure the appropriate VAD is inserted and the insertion procedure is appropriately managed using advanced techniques or technologies (1, 3, 20, 31). Advanced management is implemented at the outset and not as a rescue approach for patients with DIVA (3, 20) to maximise first insertion success (124) and reduce patient distress and discomfort (1, 21, 66). This may include the use of assistive visual technology, for example ultrasound guidance (6, 16), referral to expert vascular access clinicians (31, 95, 125) and insertion into deeper veins using longer devices (3, 126). Alternatively, CVAD insertion may be required.
Benefits of optimal DIVA management
Expert and competent management of patients with DIVA at the outset, for example using ultrasound guidance has a diverse range of benefits for the patient, clinician, and healthcare organisation compared to the unassisted, traditional, blind technique. These benefits include reduced procedural pain (14, 41, 66, 127) when compared to unassisted insertions (1, 13, 27) and reduced anxiety (1, 66). Significantly higher satisfaction in adult (40, 47), and paediatric patients and parents is also evident (128).
USG-PIVC insertion offers positive benefits for clinicians and the healthcare organisation including reduced number of unsuccessful attempts (40, 41, 67), significantly fewer attempts when compared to traditional, blind, unassisted technique (13, 47, 98). This results in reduced procedural insertion time (27, 41, 67) with statistically shorter times (13, 98) that are twice as fast as unassisted or blind insertion technique in adult patients (47). In paediatric patients, time to successful cannulation was 6-7 times faster for USG-PIVC in a randomised controlled study in operating theatre and interventional radiology (29).
Timely, successful completion of the insertion procedure minimises interruptions to overall work flow of the clinician and the department (30, 31) preventing delays in obtaining blood specimens, commencing or continuing antibiotics and other prescribed therapies (14, 28, 40). This can be facilitated by a dedicated vascular access team (31). By incorporating ultrasound guidance for PIVC insertion, prompt commencement of therapy and reduction of insertion related complications (40, 41, 96) decreases the risk of poor outcomes (30, 31). The need for alternate access is reduced, for example intraosseous or centrally inserted central catheters in emergent situations (40, 44, 54) and the documented dwell time with USG-PIVC compared to unassisted insertions was longer, 2.3 days compared to 7.3 days respectively (128). Furthermore, expenditure can be reduced with successful first insertion (40).
Early identification of paediatric patients with DIVA is also beneficial so the most appropriate management strategies can be employed to maximise first time success when there is anticipated difficulty for PIVC insertion (10). This is particularly useful for clinicians whilst building their assessment skills and proficiency in PIVC insertion (10). Paediatric patient and parental distress and anxiety is reduced with first insertion success, and by demonstrating positive outcomes from informed decision making (10).
1.2 Practice Recommendation
- 1.2.1 CNSA recommends that clinicians complete a standardised, concise venous status assessment on all patients prior to commencing intravenous therapy to pre-emptively and consistently identify adult and paediatric patients with DIVA (3, 16, 31) including:
- Vein palpability (1, 17, 20, 26, 27, 29, 35-43) GRADE IV
- Vein visibility (1, 17, 20, 26, 27, 29, 35-43) GRADE IV
- History of difficult access or use of advanced strategies to obtain vascular access (1, 13, 30, 31, 38-40, 44-52) including self-identification of their DIVA status (14, 45, 53-55) GRADE IV
- 1.2.2 CNSA recommends an evidence-based venous status assessment tool is documented in workplace procedures to standardise clinical management (40). GRADE IV
- 1.2.3 CNSA recommends a patient’s DIVA status is highlighted in a centralised location in the patient’s health record and is discussed with the patient and family for appropriate future management. GRADE CC
2. IDENTIFICATION OF PATIENTS WITH DIVA
2.1 Summary of evidence
The terms DIVA identification and DIVA prediction are used interchangeably in the literature (1, 12, 21, 22, 25, 56). Both types of tools identify similar variables, for example vein palpability and visibility, previous difficulty in venous access, medical conditions, previous intravenous therapy or the availability of one arm. However, the fundamental difference is that predictive tools are implemented prior to PIVC insertion, in order to identify patients with difficult access so advanced techniques can be employed from the outset (3, 67). Conversely, DIVA identification tools incorporate the number of failed attempts as part of the identification process and then an advanced strategy is employed (48, 54, 58, 95, 98). Also, Fiorini and colleagues (2021) developed and validated a proactive instrument for vessel health and preservation to identify patients with poor venous access using the same factors. The aim of these tools is to predict the likelihood or risk of a failed first insertion of a PIVC (1, 22) in order to prevent damage and preserve vein health for potential use in the future (7).
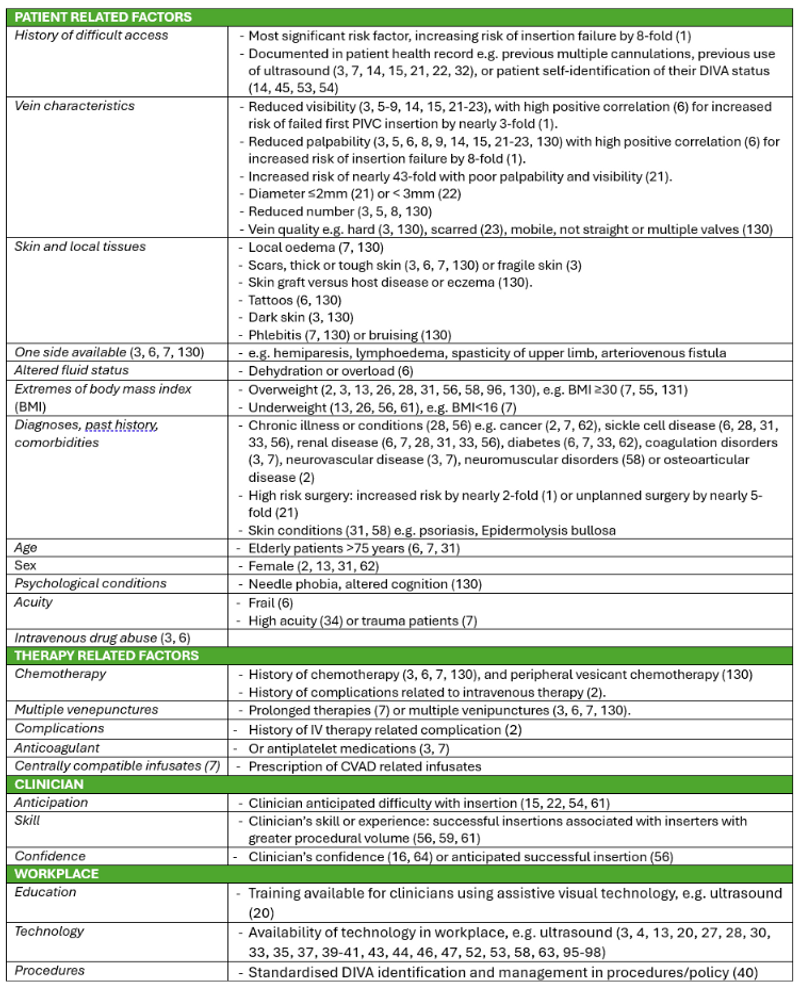
The complexity of each tool varies according to the number of variables included in the assessment, from three (12) to fifteen (7). Variables can be categorised as patient (vein characteristics, body mass index BMI, diagnoses, age, sex, acuity), therapy (previous complications, prior chemotherapy administration), clinician (experience, skill, confidence, history of failed attempts), and workplace related (training and education, equipment, and technology). Age related variables for paediatric (prematurity and age) and adult (elderly, frail) patients are also detailed. The tools include scoring systems (1, 3, 6, 10, 14, 18, 19, 21, 22, 25, 95, 129) and flow diagrams (17, 36, 99). However, the applicability of the tool for use in the clinical setting is dependent on it being simple, easy, effective and efficient (21, 25) highlighting actions required based on the outcome of the assessment.
The following section will discuss the specific variables related to adult and paediatric patients.
ADULT PATIENTS
Thirteen studies identified factors that increased risk of DIVA in the adult population. Studies included a quasi-experimental study (9); four large, observational studies (1, 3, 21, 22) and one with a Delphi component (14); three observational studies (5, 15, 23); an instrument development and validation study (7); a quality improvement study (6); survey and expert consensus (8) and a qualitative study (130).
Four types of risk factors were identified:
PAEDIATRIC PATIENTS
Early identification of paediatric patients with DIVA aims to prevent a child undergoing multiple, painful and distressing PIVC attempts. Identification and initiation of appropriate management in the first instance including appropriate technology, clinician skill and technique is required to increase first time success and improve patient comfort and outcomes (17, 18, 70, 119, 129, 132).
Seven paediatric predictive tools identified two types of predictive risk factors for unsuccessful PIVC insertion and for patients with DIVA including:
1. Patient-related factors
- Vein characteristics
- poor visibility (10, 12, 17-19, 25)
- poor palpability (10, 12, 17-19, 25)
- Younger age
- <12-18 months (10, 12, 17-19, 25, 58)
- history of prematurity (10, 12, 17-19, 25)
- History of difficult venous access: (17)
- Urgency / elective need for venous access (17)
- Diagnosis/es, medical history, comorbidity/ies
- severe comorbidities, prolonged hospital care (17)
- Skin
- dark (12)
2. Clinician-related factors
- Inserter skills (17, 19)
- Number of procedures performed (17)
- Clinician’s prediction of DIVA (57)
OTHER DEFINITIONS
Some studies referred to DIVA definitions used by researchers in published studies (11, 13, 17, 20, 26, 27, 29-31, 33-35, 37-51, 58, 62, 98, 133). These definitions identified the various contributing factors as discussed above, with the most common being (1) poor vein palpability or (2) poor vein visibility (1, 17, 20, 26, 27, 29, 35-43), and (3) history of difficult access (1, 13, 30, 31, 38-40, 44-52).
A patient with cancer can inherently experience regular and repeated PIVC insertions over the course of diagnosis, assessment, treatment, and re-evaluation of their disease status (93). However, a patient’s self-identification of their DIVA status has only relatively recently been discussed in the literature (14, 45, 53, 54). This included a patient verbalising previous difficulty with insertion, multiple attempts or insertion failure (14, 53, 54, 127, 134), or previous use of advanced strategies such as insertion by experienced clinicians or use of ultrasound (45). In a scoping review of successful cannulation in patients with DIVA by non-medical clinicians, Burton and colleagues (2022) reported DIVA assessment varied considerably in the literature and included a patient reporting a history of difficulty (54). Bahl and colleagues (2022) used a patient self-reporting their DIVA status and at least one of five other factors to identify patients with DIVA (45). Obadeyi and colleagues’ (2020) DIVA assessment included asking a patient on average how many attempts were needed to successfully cannulate their veins and to estimate the score for PIVC insertion difficulty (53). Salleras-Duran and colleagues discussed a patient’s self-identification of their DIVA status but it was not included in the DIVA tool (14). This is relevant for patients with chronic diseases such as cancer.
2.2 Practice Recommendation
- 2.2.1 CNSA recommends if a patient has at least two of the three following risks factors:
- reduced palpability or visibility of peripheral veins for the prescribed therapy, frequency and duration
- history of difficult intravenous access or self-identification of difficulty by the patient
- previous use of advanced strategies for peripheral intravenous cannula insertion documented in the health record or verbalised by the patient
- Then to proceed with:
- DIVA status is documented in the patient health record, discussed with the patient and family, and
- Proceed directly to DIVA management.
GRADE CC
- 2.2.2 CNSA recommends completing a comprehensive assessment of DIVA related factors if a clinician is uncertain or the assessment is unclear including:
- Patient related factors: patient preference, vein characteristics, body mass index, diagnoses, age, sex, acuity. NB. Age related variables for paediatric (prematurity and age) and adult (elderly, frail) patients are also detailed (2, 3, 6, 7, 10, 12, 17-19, 24-26, 28, 31, 33, 34, 56-61) GRADE IV
- Therapy related factors: prior chemotherapy administration, previous VAD related complications (2, 4, 11, 13, 20, 21, 34, 51, 57, 58, 62, 63) GRADE IV
- Clinician related factors: experience, skill, confidence (13, 16, 33, 51, 56, 59, 60, 64) GRADE IV
- Workplace related factors: training and education, equipment, and technology (20, 65, 66) GRADE IV
3. DIVA MANAGEMENT
3.1 Summary of evidence
Proactive or reactive approaches to DIVA management were evident in the included studies. The proactive approach utilized the identification tool to identify patients with DIVA and implemented advanced interventions at the outset to maximise first insertion success (3, 20, 67). Other studies detailed the number of failed attempts per clinician or total number of attempts before escalation to advanced strategies (4, 6, 10, 14-16, 48, 57, 58, 95, 97). However, to prevent patient pain and distress associated with repeated PIVC failure, appropriate clinical management for the individual patient is implemented (35, 36, 66).
Management of patients with DIVA is performed by educated, competent clinicians. Competency is associated with didactic and practical education, and the appropriate volume and frequency of procedures required by the individual clinician to develop the necessary skill and knowledge for first insertion success (17, 19, 20, 46, 56, 129). Patients identified communication, and competent and confident clinicians are important (66, 68).
ADULT PATIENTS
Management of adult patients with DIVA include:
1. Patient related management
- Education and communication regarding what to expect, to report and to whom, the risks and benefits, adequate hydration and exercise (46, 66, 68, 71)
- Preparation: alongside the venous assessment prior to commencement of intravenous therapy, patient preparation includes communication about the procedure, hydration, warmth, relaxation techniques and appropriate pain relief if required e.g. topical/subdermal anaesthesia (46, 64, 66, 68, 71-84, 91, 135)
- Post procedure: application of cold pack after the procedure for comfort if required, reinforce what to report, when and to whom, (46, 66, 68, 71)
2. Technology or product related management
- Use of imaging technology (46, 50, 57, 93) for example ultrasound increases the rate of first time success (3, 4, 13, 20, 27, 30, 33, 37, 40, 41, 43, 46, 47, 52, 53, 55, 58, 63, 95-97, 100, 136, 137) from 80% (98) to up to 93% assisted (27, 28, 35, 39, 44) when completed by a competent clinician (40). Alternatively, using a modified Seldinger Technique with ultrasound, that is using ultrasound to insert a needle into a deep vein in the arm and threading a cannula over the needle into the vein (52). First time success rate was nearly 2 (128) to 3-fold (67) with ultrasound guidance compared to unassisted insertion or standard of care, or use of NIR or IR (46, 95, 105).
3. Clinician related management
- Location
- PIVC insertion in the forearm avoiding areas of flexion (13, 110)
- Alternating arms for ongoing SACT (111)
- Attempts:
- Specified limit of the number of attempts per clinician (10, 14, 17, 48), for example 2 per nurse (6)
- Limiting the total number of IV attempts before escalation (17, 57) for example three (10, 95) or 4 (6, 58), 6 (10) in paediatric and adult patients. In a survey , 75% (n = 111) reported no limit for the total number of insertion attempts permitted in order to successfully inset at PIVC. (16)
- Referral:
- to an expert vascular access team or specialist (3, 17, 27, 31, 36, 46, 57, 95, 109, 138)
- medical staff (20, 33, 48, 63, 67) for ultrasound guidance (39, 49)
- senior clinicians (10, 13, 23, 37), for example paediatric anaesthetist with at least 5 years’ experience (95)
4. Product related:
- increased cannula length: access of deeper veins using ultrasound requires longer cannulas (6), for example 6cm (38) or 8-10 cm or a midline catheter (3, 50, 139, 140) so at least 2.7cm and ideally two thirds of the cannula resides within the vein (44, 116, 117)
- guide wire– peripheral venous cannula: to decrease the risk of puncturing the posterior vein wall, decrease trauma to the vein and ability to access deeper veins (48), a cannula with a guidewire which extended into the vein through the cannula achieved 100% success rate in patients with DIVA within three attempts (30, 43)
PAEDIATRIC PATIENTS
Management of paediatric patients with DIVA with assistive visualisation technology, for example ultrasound or NIR (29, 70, 141) and appropriate pain and anxiety management including child life specialists, distraction, virtual reality, socially-assistive robots (17, 87, 92, 118, 122, 132, 142-146).
3.2 Practice Recommendation
- 3.2.1 CNSA recommends the management of adult and paediatric patients with DIVA is performed by educated and competent clinicians (40, 66-69). GRADE IV
- 3.2.2 CNSA recommends advanced management of adults and paediatric patients with DIVA is implemented at the outset and not as a rescue strategy after failed PIVC insertion attempts (3, 20, 70). GRADE Ib
- Advanced management includes:
- Patient related: patient preparation for the procedure and care during the dwell time including -
- Education and communication regarding the procedure and dwell time, risks and benefits, what to expect, to report and to whom, and additionally in written form for (46, 66, 68, 71). GRADE IV
- Preparation: communication and education about the procedure, adequate hydration, warmth, relaxation techniques, appropriate pain and anxiety management as required e.g. topical/ subdermal anaesthesia, child life specialists, distraction, virtual reality, socially assistive robots (46, 64, 66, 68, 71-92). GRADE III
- Post procedure: application of cold pack after the procedure for comfort if required, education to reinforce what to report, when and to whom, (46, 66, 68, 71). GRADE IV
- Imaging technology:
- Use imaging technology (46, 50, 57, 93, 94) during the insertion procedure, for example
- ultrasound (3, 4, 13, 20, 27, 28, 30, 33, 35, 37, 39-41, 43, 44, 46, 47, 52, 53, 58, 63, 69, 70, 95-100) GRADE Ib OR
- NIR or IR (46, 70, 90, 95, 101-105) GRADE Ib
- Clinicians complete standardised, evidence based theoretical education and practical simulation, assessment of knowledge and practical skills, post supervised successful, independent practice attempts and competency is attained (106). GRADE IV
- Use imaging technology (46, 50, 57, 93, 94) during the insertion procedure, for example
- Clinician related:
- Referral to vascular access team or expert (3, 17, 27, 31, 36, 46, 57, 95, 107-109), for ultrasound guided insertion (39, 49) GRADE Ib
- Insertion in the forearm, avoiding areas of flexion (13, 110), alternating arms for ongoing SACTs (111). GRADE IV
- Topical application of heat prior to PIVC insertion procedure (112, 113), not for vein assessment GRADE III
- Limit the number of attempts per clinician (10, 14, 17, 48) for example:
- If after 1 failed attempt, if the clinician is not 80% confident (114) about a successful 2nd attempt, then do not proceed with 2nd attempt and escalate to more experienced vascular access clinician
- If after 1 attempt (6) and the clinician is confident in their skills and patient’s venous status, then a 2nd attempt may be made
- maximum total number of 3 IV attempts with referral to more experienced clinician (6, 10, 17, 57, 58, 95)
- paediatric patients – 0 - 2 attempts by a clinician and early referral experienced clinician (70) or PICC for ≥2 failed PIVC attempts with competent inserters and visual technology e.g. ultrasound (70) GRADE Ib
- Product related:
- Increased cannula length when deeper veins are accessed using ultrasound (3, 38, 50, 115) so at least 2.75cm and ideally two thirds of the cannula resides within the vein (44, 116, 117) (Table 2). GRADE IV
- Peripheral venous cannula with guide wire (30, 43, 48). GRADE IV
- Patient related: patient preparation for the procedure and care during the dwell time including -
For paediatric patients: consider ultrasound guided-PIVC insertion (29) and appropriate pain and anxiety management (17, 118-122) GRADE III
REFERENCES
1. Angles E, Robin F, Moal B, Roy M, Sesay M, Ouattara A, et al. Pre-operative peripheral intravenous cannula insertion failure at the first attempt in adults: Development of the VENSCORE predictive scale and identification of risk factors. Journal of clinical anesthesia. 2021;75:110435.
2. Armenteros-Yeguas V, Gárate-Echenique L, Tomás-López MA, Cristóbal-Domínguez E, Moreno-de Gusmão B, Miranda-Serrano E, et al. Prevalence of difficult venous access and associated risk factors in highly complex hospitalised patients. J Clin Nurs. 2017;26(23-24):4267-75.
3. Civetta G, Cortesi S, Mancardi M, De Pirro A, Vischio M, Mazzocchi M, et al. EA-DIVA score (Enhanced Adult DIVA score): A new scale to predict difficult preoperative venous cannulation in adult surgical patients. The journal of vascular access. 2019;20(3):281-9.
4. Davis EM, Feinsmith S, Amick AE, Sell J, McDonald V, Trinquero P, et al. Difficult intravenous access in the emergency department: Performance and impact of ultrasound-guided IV insertion performed by nurses. Am J Emerg Med. 2021;46:539-44.
5. de la Torre-Montero J-C, Montealegre-Sanz M, Faraldo-Cabana A, Oliva-Pellicer B, Garcia-Real I, Fenwick M, et al. Venous International Assessment, VIA scale, validated classification procedure for the peripheral venous system. The journal of vascular access. 2014;15(1):45-50.
6. Ehrhardt BS, Givens KEA, Lee RC. Making It Stick: Developing and Testing the Difficult Intravenous Access (DIVA) Tool. The American journal of nursing. 2018;118(7):56-62.
7. Fiorini J, Piredda M, Zaghini F, Venturini G, Colella S, Conti F, et al. Vessel health and preservation: Development and validation of a proactive instrument. Collegian. 2021;28(5):528-33.
8. Magallon-Pedrera I, Perez-Altozano J, Virizuela Echaburu JA, Beato-Zambrano C, Borrega-Garcia P, de la Torre-Montero JC. ECO-SEOM-SEEO safety recommendations guideline for cancer patients receiving intravenous therapy. Clinical & translational oncology : official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico. 2020;22(11):2049-60.
9. Moondeep K, Anil K, Anshul D. Effect of Moist Heat Therapy on the Visibility and Palpability of Peripheral Veins Before Peripheral Venous Cannulation among Patients Undergoing Intravenous Cannulation- A Quasi Experimental Study. International Journal of Nursing Care. 2020;8(2):Oct-14.
10. O'Neill MB, Dillane M, Hanipah NF. Validating the difficult intravenous access clinical prediction rule. Pediatric Emergency Care. 2012;28(12):1314-6.
11. Pagnutti L, Bin A, Donato R, Di Lena G, Fabbro C, Fornasiero L, et al. Difficult intravenous access tool in patients receiving peripheral chemotherapy: A pilot-validation study. European journal of oncology nursing : the official journal of European Oncology Nursing Society. 2016;20:58-63.
12. Riker MW, Kennedy C, Winfrey BS, Yen K, Dowd MD. Validation and refinement of the difficult intravenous access score: a clinical prediction rule for identifying children with difficult intravenous access. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2011;18(11):1129-34.
13. Rodriguez-Calero MA, de Pedro-Gomez JE, Molero-Ballester LJ, Fernandez-Fernandez I, Matamalas-Massanet C, Moreno-Mejias L, et al. Risk Factors for Difficult Peripheral Intravenous Cannulation. The PIVV2 Multicentre Case-Control Study. Journal of clinical medicine. 2020;9(3).
14. Salleras-Duran L, Fuentes-Pumarola C, Ballester-Ferrando D, Congost-Devesa L, Delclos-Rabassa J, Fontova-Almato A. Development, Diagnostic Sensitivity, and Prognostic Accuracy of the Adult-Difficult Venous Catheterization Scale for Emergency Departments. Journal of emergency nursing. 2020;46(6):827-37.e2.
15. Santos-Costa P, Sousa LB, van Loon FHJ, Salgueiro-Oliveira A, Parreira P, Vieira M, et al. Translation and Validation of the Modified A-DIVA Scale to European Portuguese: Difficult Intravenous Access Scale for Adult Patients. International journal of environmental research and public health. 2020;17(20).
16. Schults J, Rickard C, Kleidon T, Paterson R, Macfarlane F, Ullman A. Difficult Peripheral Venous Access in Children: An International Survey and Critical Appraisal of Assessment Tools and Escalation Pathways. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing. 2019;51(5):537-46.
17. Schults JA, Kleidon TM, Gibson V, Ware RS, Monteagle E, Paterson R, et al. Improving peripheral venous cannula insertion in children: a mixed methods study to develop the DIVA key. BMC health services research. 2022;22(1):220.
18. Shaukat H, Neway B, Breslin K, Watson A, Poe K, Boniface K, et al. Utility of the DIVA score for experienced emergency department technicians. British journal of nursing (Mark Allen Publishing). 2020;29(2):S35-S40.
19. Suchitra E, Srinivasan R. Effectiveness of dry heat application on ease of venepuncture in children with difficult intravenous access: A randomized controlled trial. Journal for specialists in pediatric nursing : JSPN. 2020;25(1):e12273.
20. Sweeny A, Archer-Jones A, Watkins S, Johnson L, Gunter A, Rickard C. The experience of patients at high risk of difficult peripheral intravenous cannulation: An Australian prospective observational study. Australasian emergency care. 2022;25(2):140-6.
21. Van Loon FHJ, Puijn LAPM, Houterman S, Bouwman ARA, Loon FHJv. Development of the A-DIVA Scale: A Clinical Predictive Scale to Identify Difficult Intravenous Access in Adult Patients Based on Clinical Observations. Medicine. 2016;95(16):1-Aug.
22. van Loon FHJ, van Hooff LWE, de Boer HD, Koopman SSHA, Buise MP, Korsten HHM, et al. The Modified A-DIVA Scale as a Predictive Tool for Prospective Identification of Adult Patients at Risk of a Difficult Intravenous Access: A Multicenter Validation Study. Journal of clinical medicine. 2019;8(2).
23. Webster J, Morris H, Robinson K, Sanderson U. Development and validation of a Vein Assessment Tool (VAT). Australian Journal of Advanced Nursing. 2007;24(4):5-Jul.
24. Wells S. Venous access in oncology and haematology patients: Part one. Nursing standard (Royal College of Nursing (Great Britain) : 1987). 2008;22(52):39-46.
25. Yen K, Riegert A, Gorelick MH. Derivation of the DIVA score: a clinical prediction rule for the identification of children with difficult intravenous access. Pediatr Emerg Care. 2008;24(3):143-7.
26. Sebbane M, Claret PG, Lefebvre S, Mercier G, Rubenovitch J, Jreige R, et al. Predicting peripheral venous access difficulty in the emergency department using body mass index and a clinical evaluation of venous accessibility. J Emerg Med. 2013;44(2):299-305.
27. Sou V, McManus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16:64.
28. Brannam L, Blaivas M, Lyon M, Flake M. Emergency nurses' utilization of ultrasound guidance for placement of peripheral intravenous lines in difficult-access patients. Academic Emergency Medicine. 2004;11(12):1361-3.
29. Benkhadra M, Collignon M, Fournel I, Oeuvrard C, Rollin P, Perrin M, et al. Ultrasound guidance allows faster peripheral IV cannulation in children under 3 years of age with difficult venous access: a prospective randomized study. Paediatr Anaesth. 2012;22(5):449-54.
30. Raio C, Elspermann R, Kittisarapong N, Stankard B, Bajaj T, Modayil V, et al. A prospective feasibility trial of a novel intravascular catheter system with retractable coiled tip guidewire placed in difficult intravascular access (DIVA) patients in the Emergency Department. Internal and emergency medicine. 2018;13(5):757-64.
31. Whalen M, Maliszewski B, Sheinfeld R, Gardner H, Baptiste D. Outcomes of an Innovative Evidence-Based Practice Project: Building a Difficult-Access Team in the Emergency Department. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2018;44(5):478-82.
32. Witting MD. IV access difficulty: incidence and delays in an urban emergency department. J Emerg Med. 2012;42(4):483-7.
33. Fields JM, Piela NE, Au AK, Ku BS. Risk factors associated with difficult venous access in adult ED patients. Am J Emerg Med. 2014;32(10):1179-82.
34. Heydinger G, Shafy SZ, O'Connor C, Nafiu O, Tobias JD, Beltran RJ. Characterization of the Difficult Peripheral IV in the Perioperative Setting: A Prospective, Observational Study of Intravenous Access for Pediatric Patients Undergoing Anesthesia. Pediatric health, medicine and therapeutics. 2022;13:155-63.
35. Hallam C, Denton A. Vessel health and preservation 1: minimising the risks of vascular access. Nursing Times. 2020;116(7):22-5.
36. Hallam C, Denton A, Weston V, Dunn H, Jackson T, Keeling S, et al. UK Vessel Health and Preservation (VHP) Framework: a commentary on the updated VHP 2020. Journal of infection prevention. 2021;22(4):147-55.
37. Hallam C, Jackson T, Weston V, Denton A, Hill S, Bodenham A, et al. Development of the UK Vessel Health and Preservation (VHP) framework: a multi-organisational collaborative. Journal of Infection Prevention. 2016;17(2):65-72.
38. Brugioni L, Barchetti M, Tazzioli G, Gelmini R, Girardis M, Bianchini M, et al. A new device for ultrasound-guided peripheral venous access. The journal of vascular access. 2019;20(3):325-8.
39. Costantino TG, Kirtz JF, Satz WA. Ultrasound-guided peripheral venous access vs. the external jugular vein as the initial approach to the patient with difficult vascular access. J Emerg Med. 2010;39(4):462-7.
40. Lamperti M, Biasucci DG, N DI, Pittiruti M, Breschan C, Vailati D, et al. European Society of Anaesthesiology guidelines on peri-operative use of ultrasound-guided for vascular access (PERSEUS vascular access). European Journal of Anaesthesiology. 2020;37(5):344-76.
41. Rodriguez-Herrera A, Solaz-Garcia A, Molla-Olmos E, Ferrer-Puchol D, Esteve-Claramunt F, Trujillo-Barbera S, et al. Use of the Ultrasound Technique as Compared to the Standard Technique for the Improvement of Venous Cannulation in Patients with Difficult Access. Healthcare (Basel, Switzerland). 2022;10(2).
42. Santos-Costa P, Paiva-Santos F, Sousa LB, Bernardes RA, Ventura F, Fearnley WD, et al. Nurses' Practices in the Peripheral Intravenous Catheterization of Adult Oncology Patients: A Mix-Method Study. Journal of personalized medicine. 2022;12(2).
43. Scoppettuolo G, Pittiruti M, Pitoni S, Dolcetti L, Emoli A, Mitidieri A, et al. Ultrasound-guided short midline catheters for difficult venous access in the emergency department: a retrospective analysis. International journal of emergency medicine. 2016;9(1):3.
44. Blanco P. Ultrasound-guided peripheral venous cannulation in critically ill patients: a practical guideline. The ultrasound journal. 2019;11(1):27.
45. Bahl A, Hijazi M, Chen NW. Vesicant infusates are not associated with ultrasound-guided peripheral intravenous catheter failure: A secondary analysis of existing data. PLoS ONE. 2022;17(1-Jan):e0262793.
46. Barth D, Sanchez A, Thomsen A-M, Garcia A, Malachowski R, Weldon R, et al. Peripheral vascular access for therapeutic plasma exchange: A practical approach to increased utilization and selecting the most appropriate vascular access. Journal of clinical apheresis. 2020;35(3):178-87.
47. Bauman M, Braude D, Crandall C. Ultrasound-guidance vs. standard technique in difficult vascular access patients by ED technicians. The American journal of emergency medicine. 2009;27(2):135-40.
48. Chiricolo G, Balk A, Raio C, Wen W, Mihailos A, Ayala S. Higher success rates and satisfaction in difficult venous access patients with a guide wire-associated peripheral venous catheter. The American journal of emergency medicine. 2015;33(12):1742-4.
49. Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Annals of emergency medicine. 2005;46(5):456-61.
50. Fabiani A, Eletto V, Dreas L, Beltrame D, Sanson G. Midline or long peripheral catheters in difficult venous access conditions? A comparative study in patients with acute cardiovascular diseases. American journal of infection control. 2020;48(10):1158-65.
51. Witting MD, Moayedi S, Hirshon JM, George NH, Schenkel SM. Predicting Failure of Intravenous Access in Adults: The Value of Prior Difficulty. J Emerg Med. 2019;57(1):1-5.
52. Warrington Jr WG, Penoyer DA, Kamps TA, Van Hoeck EH. Outcomes of using a modified seldinger technique for long term intravenous therapy in hospitalized patients with difficult venous access. JAVA - Journal of the Association for Vascular Access. 2012;17(1):24-30.
53. Obadeyi O, Baffoe N, Paxton J. A patient's decision aid for vascular access placement in the emergency department. The journal of vascular access. 2020;21(4):419-25.
54. Burton SO, Donovan JK, Jones SL, Meadley BN. Can Non-Physician Providers Use Ultrasound to Aid in Establishing Peripheral IV Access in Patients Who are Difficult to Cannulate? A Scoping Review. Prehospital and disaster medicine. 2022;37(4):535-46.
55. Schoenfeld E, Shokoohi H, Boniface K. Ultrasound-guided peripheral intravenous access in the emergency department: patient-centered survey. The western journal of emergency medicine. 2011;12(4):475-7.
56. Carr PJ, Higgins NS, Cooke ML, Rippey J, Rickard CM. Tools, Clinical Prediction Rules, and Algorithms for the Insertion of Peripheral Intravenous Catheters in Adult Hospitalized Patients: A Systematic Scoping Review of Literature. Journal of hospital medicine. 2017;12(10):851-8.
57. Girotto C, Arpone M, Frigo AC, Micheletto M, Mazza A, Da Dalt L, et al. External validation of the DIVA and DIVA3 clinical predictive rules to identify difficult intravenous access in paediatric patients. Emergency medicine journal : EMJ. 2020;37(12):762-7.
58. Hakim M, Shafy SZ, Uffman JC, Rice J, Raman VT, Tobias JD, et al. A Survey to Define and Predict Difficult Vascular Access in the Pediatric Perioperative Population. Pediatric health, medicine and therapeutics. 2020;11:277-82.
59. Lee SU, Jung JY, Ham EM, Wang SW, Park JW, Hwang S, et al. Factors associated with difficult intravenous access in the pediatric emergency department. The journal of vascular access. 2020;21(2):180-5.
60. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community Emergency Department. J Vasc Access. 2015;16(6):521-6.
61. Carr PJ, Rippey JC, Budgeon CA, Cooke ML, Higgins N, Rickard CM. Insertion of peripheral intravenous cannulae in the Emergency Department: factors associated with first-time insertion success. J Vasc Access. 2016;17(2):182-90.
62. Piredda M, Biagioli V, Barrella B, Carpisassi I, Ghinelli R, Giannarelli D, et al. Factors affecting difficult peripheral intravenous cannulation in adults: a prospective observational study. Journal of clinical nursing. 2017;26(7-Aug):1074-84.
63. Weiner SG, Sarff AR, Esener DE, Shroff SD, Budhram GR, Switkowski KM, et al. Single-operator ultrasound-guided intravenous line placement by emergency nurses reduces the need for physician intervention in patients with difficult-to-establish intravenous access. The Journal of emergency medicine. 2013;44(3):653-60.
64. Farrell C, McCulloch E, Bellhouse S, Delahoyde M-K, Hill S, Rickard C, et al. Peripheral cannulae in oncology: nurses' confidence and patients' experiences. Cancer Nursing Practice. 2017;16(3):32-8.
65. Morrell E. Reducing Risks and Improving Vascular Access Outcomes. Journal of infusion nursing : the official publication of the Infusion Nurses Society. 2020;43(4):222-8.
66. Plohal A. A Qualitative Study of Adult Hospitalized Patients With Difficult Venous Access Experiencing Short Peripheral Catheter Insertion in a Hospital Setting. Journal of infusion nursing : the official publication of the Infusion Nurses Society. 2021;44(1):26-33.
67. Bahl A, Pandurangadu AV, Tucker J, Bagan M. A randomized controlled trial assessing the use of ultrasound for nurse-performed IV placement in difficult access ED patients. Am J Emerg Med. 2016;34(10):1950-4.
68. Cuthbertson L, Ashton S. The patient experience of peripheral intravenous therapy: development of a patient survey, initial findings, and next steps. British journal of nursing (Mark Allen Publishing). 2021;30(2):S42-S8.
69. Steere L, Ficara C, Davis M, Moureau N. Reaching One Peripheral Intravenous Catheter (PIVC) Per Patient Visit With Lean Multimodal Strategy: the PIV5Rights™ Bundle. Journal of the Association for Vascular Access. 2019;24(3):31-43.
70. Ullman AJ, Bernstein SJ, Brown E, Aiyagari R, Doellman D, Faustino EVS, et al. The Michigan Appropriateness Guide for Intravenous Catheters in Pediatrics: miniMAGIC. Pediatrics. 2020;145(Suppl 3):S269-S84.
71. Colucci N, Gregoris A, Meyer J, Naiken SP, Staszewicz W, Gialamas E, et al. Introduction of a specialized consultation prior to insertion of totally implantable access venous devices: Impact on cancellation rate and patient satisfaction. Vascular. 2020;28(6):816-20.
72. Agarwal A, Sinha PK, Tandon M, Dhiraaj S, Singh U. Evaluating the efficacy of the Valsalva maneuver on venous cannulation pain: A prospective, randomized study. Anesthesia and Analgesia. 2005;101(4):1230-2.
73. Agarwal A, Yadav G, Gupta D, Tandon M, Dhiraaj S, Singh PK. Comparative evaluation of myolaxin and EMLA cream for attenuation of venous cannulation pain: a prospective, randomised, double blind study. Anaesthesia and intensive care. 2007;35(5):726-9.
74. Agarwal A, Gautam S, Gupta D, Singh U. Transdermal diclofenac patch vs eutectic mixture of local anesthetics for venous cannulation pain. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2007;54(3):196-200.
75. Alobayli FY. Factors Influencing Nurses' Use of Local Anesthetics for Venous and Arterial Access. Journal of infusion nursing : the official publication of the Infusion Nurses Society. 2019;42(2):91-107.
76. Anderson S, Cockrell J, Beller P, Murphy E, Nelson P, Hawkins M, et al. Administration of local anesthetic agents to decrease pain associated with peripheral vascular access. Journal of Infusion Nursing. 2010;33(6):353-61.
77. Basak T, Duman S, Demirtas A. Distraction-based relief of pain associated with peripheral intravenous catheterisation in adults: a randomised controlled trial. Journal of clinical nursing. 2020;29(5-Jun):770-7.
78. Basaranoglu G, Basaranoglu M, Erden V, Delatioglu H, Pekel AF, Saitoglu L. The effects of Valsalva manoeuvres on venepuncture pain. European Journal of Anaesthesiology. 2006;23(7):591-3.
79. Brown J. Using lidocaine for peripheral i.v. insertions: patients' preferences and pain experiences. Medsurg nursing : official journal of the Academy of Medical-Surgical Nurses. 2003;12(2):95-101.
80. Brown D. Local anesthesia for vein cannulation: a comparison of two solutions. Journal of infusion nursing : the official publication of the Infusion Nurses Society. 2004;27(2):85-8.
81. Burton KLO, Morrow AM, Beswick BV, Khut GP. The Feasibility of Using the BrightHearts Biofeedback?Assisted Relaxation Application for the Management of Pediatric Procedural Pain: A Pilot Study. Pain Practice. 2018;18(8):979-87.
82. Caruso TJ, George A, Menendez M, De Souza E, Khoury M, Kist MN, et al. Virtual reality during pediatric vascular access: A pragmatic, prospective randomized, controlled trial. Paediatric anaesthesia. 2020;30(2):116-23.
83. Edwards C, Noah C. A Randomized, Double-Blind Trial to Determine if Vapocoolant in the Adult Population Improves Patient Perception of Pain With Peripheral Intravascular Access. Advanced emergency nursing journal. 2017;39(4):288-94.
84. Mace SE. Prospective, double blind, randomized, controlled trial comparing vapocoolant spray versus placebo spray in adults undergoing intravenous cannulation. Scandinavian journal of pain. 2017;17:Aug-15.
85. Fusco N, Bernard F, Roelants F, Watremez C, Musellec H, Laviolle B, et al. Hypnosis and communication reduce pain and anxiety in peripheral intravenous cannulation: Effect of Language and Confusion on Pain During Peripheral Intravenous Catheterization (KTHYPE), a multicentre randomised trial. BJA: The British Journal of Anaesthesia. 2020;124(3):292-8.
86. Hall DL, Rezvan E, Tatakis DN, Walters JD. Oral clonidine pretreatment prior to venous cannulation. Anesthesia progress. 2006;53(2):34-42.
87. McCollum NL, Kamat PP, Stockwell JA, Travers C, McCracken CE, Thompson B, et al. Improving Stakeholder Satisfaction: Nitrous Oxide for Peripheral Intravenous Cannulation for Pediatric Procedural Sedation. Journal of Radiology Nursing. 2017;36(4):238-41.
88. McGowan D. Peripheral intravenous cannulation: managing distress and anxiety. British Journal of Nursing. 2014;23:S4-S9.
89. Ragg PG, Cahoon G, Yeo A, Chalkiadis G. A clinical audit to assess the efficacy of the Coolsense R Pain Numbing Applicator for intravenous cannulation in children. Anaesthesia and intensive care. 2017;45(2):251-5.
90. Ramer L, Hunt P, Ortega E, Knowlton J, Briggs R, Hirokawa S. Effect of Intravenous (IV) Assistive Device (VeinViewer) on IV Access Attempts, Procedural Time, and Patient and Nurse Satisfaction. Journal of pediatric oncology nursing : official journal of the Association of Pediatric Oncology Nurses. 2016;33(4):273-81.
91. Waterhouse MR, Liu DR, Wang VJ. Cryotherapeutic topical analgesics for pediatric intravenous catheter placement: Ice versus vapocoolant spray. Pediatric Emergency Care. 2013;29(1):8-Dec.
92. Wong CL, Li CK, Chan CWH, Choi KC, Chen J, Yeung MT, et al. Virtual Reality Intervention Targeting Pain and Anxiety Among Pediatric Cancer Patients Undergoing Peripheral Intravenous Cannulation: A Randomized Controlled Trial. Cancer Nursing. 2021;44(6):435-42.
93. Eren H, Caliskan N. Effect of a Vein Imaging Device and of Fist Clenching on Determination of an Appropriate Vein and on Catheter Placement Time in Patients Receiving Chemotherapy: A Randomized Controlled Trial. Cancer nursing. 2022;45(2):105-12.
94. Usclade A, Blanc N, Kohlmuller M, Torres A, Siret S, Tachet C, et al. Infrared augmented reality device versus standard procedure for peripheral venous catheterisation in children less than 3 years old: A quasi-experimental cluster randomised controlled trial. Journal of clinical nursing. 2022;31(11-Dec):1628-35.
95. de Graaff JC, Cuper NJ, van Dijk AT, Timmers-Raaijmaakers BC, van der Werff DB, Kalkman CJ. Evaluating NIR vascular imaging to support intravenous cannulation in awake children difficult to cannulate; a randomized clinical trial. Paediatr Anaesth. 2014;24(11):1174-9.
96. Maiocco G, Coole C. Use of Ultrasound Guidance for Peripheral Intravenous Placement in Difficult-to-Access Patients: Advancing Practice With Evidence. Journal of Nursing Care Quality. 2012;27(1):51-5.
97. Schults JA, Calleja P, Slaughter E, Paterson R, Rickard CM, Booker C, et al. Peripheral intravenous catheter insertion and use of ultrasound in patients with difficult intravenous access: Australian patient and practitioner perspectives to inform future implementation strategies. PloS one. 2022;17(6):e0269788.
98. Doniger SJ, Ishimine P, Fox JC, Kanegaye JT. Randomized controlled trial of ultrasound-guided peripheral intravenous catheter placement versus traditional techniques in difficult-access pediatric patients. Pediatr Emerg Care. 2009;25(3):154-9.
99. Kanno C, Murayama R, Abe-Doi M, Takahashi T, Shintani Y, Nogami J, et al. Development of an algorithm using ultrasonography-assisted peripheral intravenous catheter placement for reducing catheter failure. Drug discoveries & therapeutics. 2020;14(1):27-34.
100. Nishizawa T, Matsumoto T, Todaka T, Sasano M, Kitagawa H, Shimabuku A. Nurse-Performed Ultrasound-Guided Technique for Difficult Peripheral Intravenous Access in Critically Ill Patients: A Randomized Controlled Trial. Journal of the Association for Vascular Access. 2020;25(2):34-9.
101. Bayram D, Topan A. The efficiency of vein viewing on pain and anxiety of children during peripheral cannula intervention: A randomized controlled study. Japan journal of nursing science : JJNS. 2020;17(4):e12364.
102. Chapman LL, Sullivan B, Pacheco AL, Draleau CP, Becker BM. VeinViewer-assisted Intravenous catheter placement in a pediatric emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2011;18(9):966-71.
103. Kim MJ, Park JM, Rhee N, Je SM, Hong SH, Lee YM, et al. Efficacy of VeinViewer in pediatric peripheral intravenous access: a randomized controlled trial. European journal of pediatrics. 2012;171(7):1121-5.
104. Perry AM, Caviness AC, Hsu DC. Efficacy of a near-infrared light device in pediatric intravenous cannulation: a randomized controlled trial. Pediatric emergency care. 2011;27(1):5-Oct.
105. Zhang Z, Wang X, Zhang L, Lou X, Su X, Wang X, et al. Infrared Vein Imaging for Insertion of Peripheral Intravenous Catheter for Patients Requiring Isolation for Severe Acute Respiratory Syndrome Coronavirus 2 Infection: A Nonrandomized Clinical Trial. Journal of emergency nursing. 2022;48(2):159-66.
106. Nickel B, Gorski LA, M. KT, Kyes A, DeVries M, Keogh S, et al. Infusion therapy standards of practice. J Infus Nurs. 2024;47 (suppl1):S1-S285.
107. Fujioka G, Newcomb P, Hunchusky C, Myers H, Behan D. Pain Perception of a Structured Vascular Access Team Approach to Short Peripheral Catheter (SPC) Placement Compared to SPC Placement by Bedside Nurses. Journal of infusion nursing : the official publication of the Infusion Nurses Society. 2020;43(1):33-8.
108. Marsh N, Webster J, Larsen E, Genzel J, Cooke M, Mihala G, et al. Expert versus generalist inserters for peripheral intravenous catheter insertion: a pilot randomised controlled trial. Trials. 2018;19(1):564.
109. McGowan D, Wood S. Developing a venous assessment tool in IV chemotherapy administration. British journal of nursing (Mark Allen Publishing). 2008;17(3):158-64.
110. Murayama R, Takahashi T, Tanabe H, Yabunaka K, Oe M, Komiyama C, et al. Exploring the causes of peripheral intravenous catheter failure based on shape of catheters removed from various insertion sites. Drug discoveries & therapeutics. 2018;12(3):170-7.
111. Roberts R, Hanna L, Borley A, Dolan G, Williams EM. Epirubicin chemotherapy in women with breast cancer: Alternating arms for intravenous administration to reduce chemical phlebitis. European journal of cancer care. 2019;28(5):e13114.
112. Korkut S, Karadag S, Dogan Z. The Effectiveness of Local Hot and Cold Applications on Peripheral Intravenous Catheterization: A Randomized Controlled Trial. Journal of perianesthesia nursing : official journal of the American Society of PeriAnesthesia Nurses. 2020;35(6):597-602.
113. Lenhardt R, Seybold T, Kimberger O, Stoiser B, Sessler DI. Local warming and insertion of peripheral venous cannulas: single blinded prospective randomised controlled trial and single blinded randomised crossover trial. BMJ (Clinical research ed). 2002;325(7361):409-10.
114. Carr PJ, Rippey JCR, Cooke ML, Higgins NS, Trevenen ML, Foale A, et al. Derivation of a clinical decision-making aid to improve the insertion of clinically indicated peripheral intravenous catheters and promote vessel health preservation. An observational study. PloS one. 2019;14(3):e0213923.
115. Meyer BM. Making the Most of Midlines: A Retrospective Review of Outcomes. Journal of infusion nursing : the official publication of the Infusion Nurses Society. 2020;43(6):344-50.
116. Pandurangadu AV, Tucker J, Brackney AR, Bahl A. Ultrasound-guided intravenous catheter survival impacted by amount of catheter residing in the vein. Emerg Med J. 2018;35(9):550-5.
117. Bahl A, Hijazi M, Chen NW, Lachapelle-Clavette L, Price J. Ultralong Versus Standard Long Peripheral Intravenous Catheters: A Randomized Controlled Trial of Ultrasonographically Guided Catheter Survival. Ann Emerg Med. 2020;76(2):134-42.
118. Clark ME, Carleton ME, Cummings BM, Noviski N. Children's drawings with narratives in the hospital setting: Insights into the patient experience. Hospital Pediatrics. 2019;9(7):495-500.
119. Costello M, Ramundo M, Christopher NC, Powell KR. Ethyl vinyl chloride vapocoolant spray fails to decrease pain associated with intravenous cannulation in children. Clinical Pediatrics. 2006;45(7):628-32.
120. Kearl YL, Yanger S, Montero S, Morelos-Howard E, Claudius I. Does Combined Use of the J-tip® and Buzzy® Device Decrease the Pain of Venipuncture in a Pediatric Population? Journal of Pediatric Nursing. 2015;30(6):829-33.
121. Stoltz P, Manworren RCB. Comparison of Children's Venipuncture Fear and Pain: Randomized Controlled Trial of EMLA® and J-Tip Needleless Injection System®. J Pediatr Nurs. 2017;37:91-6.
122. Trost MJ, Chrysilla G, Gold JI, Mataric M. Socially-Assistive Robots Using Empathy to Reduce Pain and Distress during Peripheral IV Placement in Children. Pain Research and Management. 2020;2020:7935215.
123. Robinson-Reilly M, Paliadelis P, Cruickshank M. Venous access: the patient experience. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2016;24(3):1181-7.
124. Australian Commission on Safety and Quality in Health Care. Management of Peripheral Intravenous Catheters Clinical Care Standard. In: Australian Commission on Safety and Quality in Health Care, editor. Sydney2021.
125. Corcuera Martinez MI, Aldonza Torres M, Diez Revilla AM, Maali Centeno S, Maneru Oria A, Elizari Roncal I, et al. Impact assessment following implementation of a vascular access team. The journal of vascular access. 2022;23(1):135-44.
126. Elia F, Ferrari G, Molino P, Converso M, De Filippi G, Milan A, et al. Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. The American journal of emergency medicine. 2012;30(5):712-6.
127. Fields JM, Piela NE, Ku BS. Association between multiple IV attempts and perceived pain levels in the emergency department. The journal of vascular access. 2014;15(6):514-8.
128. Vinograd AM, Chen AE, Woodford AL, Fesnak S, Gaines S, Elci OU, et al. Ultrasonographic Guidance to Improve First-Attempt Success in Children With Predicted Difficult Intravenous Access in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2019;74(1):19-27.
129. Hartman JH, Bena JF, Morrison SL, Albert NM. Criterion and Construct Validity and Reliability of the Pediatric IV Difficulty Score. Journal of the Association for Vascular Access. 2020;25(3):40-4.
130. Wells S. Venous access in oncology and haematology patients: Part two. Nurs Stand. 2008;23(1):35-42.
131. Brusasco C, Corradi F, Zattoni PL, Launo C, Leykin Y, Palermo S. Ultrasound-guided central venous cannulation in bariatric patients. Obesity surgery. 2009;19(10):1365-70.
132. Cozzi G, Valerio P, Kennedy R. A narrative review with practical advice on how to decrease pain and distress during venepuncture and peripheral intravenous cannulation. Acta paediatrica (Oslo, Norway : 1992). 2021;110(2):423-32.
133. Piredda M, Fiorini J, Facchinetti G, Biagioli V, Marchetti A, Conti F, et al. Risk factors for a difficult intravenous access: A multicentre study comparing nurses' beliefs to evidence. Journal of clinical nursing. 2019;28(19-20):3492-504.
134. Larsen E, Keogh S, Marsh N, Rickard C. Experiences of peripheral IV insertion in hospital: a qualitative study. British journal of nursing (Mark Allen Publishing). 2017;26(19):S18-S25.
135. Suren M, Kaya Z, Ozkan F, Erkorkmaz U, Arici S, Karaman S. Comparison of the use of the Valsalva maneuver and the eutectic mixture of local anesthetics (EMLA R) to relieve venipuncture pain: a randomized controlled trial. Journal of anesthesia. 2013;27(3):407-11.
136. Moureau NL, Trick N, Nifong T, Perry C, Kelley C, Carrico R, et al. Vessel health and preservation (Part 1): a new evidence-based approach to vascular access selection and management. J Vasc Access. 2012;13(3):351-6.
137. Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, et al. Guidelines for performing ultrasound guided vascular cannulation: Recommendations of the American society of echocardiography and the society of cardiovascular anesthesiologists. Anesthesia and Analgesia. 2012;114(1):46-72.
138. Golden S, Weaver J, Russell E, Park B, Sowa P, Blecha M. Educational Value of an Intern-Directed Vascular Access Team at a Community Teaching Hospital. American Surgeon. 2022;88(6):1159-62.
139. Gilardi E, Giannuzzi R, WoldeSellasie K, Piano A, Pittiruti M, Scoppettuolo G. Mini-midline in difficult intravenous access patients in emergency department: A prospective analysis. J Vasc Access. 2020;21(4):449-55.
140. Lescinskas EH, Trautner BW, Saint S, Colozzi J, Evertsz K, Chopra V, et al. Use of and patient-reported complications related to midline catheters and peripherally inserted central catheters. Infection control and hospital epidemiology. 2020;41(5):608-10.
141. Takeshita J, Nakayama Y, Nakajima Y, Sessler DI, Ogawa S, Sawa T, et al. Optimal site for ultrasound-guided venous catheterisation in paediatric patients: an observational study to investigate predictors for catheterisation success and a randomised controlled study to determine the most successful site. Critical care (London, England). 2015;19:15.
142. Goldman RD, Behboudi A. Virtual reality for intravenous placement in the emergency department-a randomized controlled trial. European Journal of Pediatrics. 2021;180(3):725-31.
143. Murag S, Suzukawa C, Chang TP. The Effects of Child Life Specialists on Success Rates of Intravenous Cannulation. Journal of pediatric nursing. 2017;36:236-40.
144. Nilsson S, Finnström B, Kokinsky E, Enskär K. The use of Virtual Reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. European Journal of Oncology Nursing. 2009;13(2):102-9.
145. Walther-Larsen S, Petersen T, Friis SM, Aagaard G, Drivenes B, Opstrup P. Immersive Virtual Reality for Pediatric Procedural Pain: A Randomized Clinical Trial. Hospital pediatrics. 2019;9(7):501-7.
146. Wang E, Thomas JJ, Rodriguez ST, Kennedy KM, Caruso TJ. Virtual reality for pediatric periprocedural care. Current opinion in anaesthesiology. 2021;34(3):284-91.
